Fexinidazole
Description
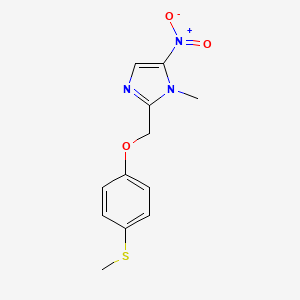
Fexinidazole is an orally administered 5-nitroimidazole prodrug developed for treating Human African Trypanosomiasis (HAT) and investigated for visceral leishmaniasis (VL) and Chagas disease. Discovered in the 1970s and revitalized by the Drugs for Neglected Diseases initiative (DNDi), it undergoes hepatic metabolism to two active metabolites: this compound sulfoxide (M1) and this compound sulfone (M2). These metabolites exhibit trypanocidal and leishmanicidal activities comparable to the parent compound .
This compound demonstrates broad-spectrum activity against Trypanosoma brucei (both gambiense and rhodesiense), curing acute and chronic murine models at 100 mg/kg twice daily for 5 days . It achieves brain concentrations exceeding IC50 values, critical for treating stage 2 HAT (CNS involvement) . Despite mutagenicity in bacterial Ames tests, it lacks genotoxicity in mammalian assays, enabling clinical development .
Properties
IUPAC Name |
1-methyl-2-[(4-methylsulfanylphenoxy)methyl]-5-nitroimidazole | |
|---|---|---|
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI |
InChI=1S/C12H13N3O3S/c1-14-11(13-7-12(14)15(16)17)8-18-9-3-5-10(19-2)6-4-9/h3-7H,8H2,1-2H3 | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI Key |
MIWWSGDADVMLTG-UHFFFAOYSA-N | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Canonical SMILES |
CN1C(=CN=C1COC2=CC=C(C=C2)SC)[N+](=O)[O-] | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Molecular Formula |
C12H13N3O3S | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
DSSTOX Substance ID |
DTXSID00208448 | |
| Record name | Fexinidazole | |
| Source | EPA DSSTox | |
| URL | https://comptox.epa.gov/dashboard/DTXSID00208448 | |
| Description | DSSTox provides a high quality public chemistry resource for supporting improved predictive toxicology. | |
Molecular Weight |
279.32 g/mol | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Solubility |
Practically insoluble | |
| Record name | Fexinidazole | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB12265 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
CAS No. |
59729-37-2 | |
| Record name | Fexinidazole | |
| Source | CAS Common Chemistry | |
| URL | https://commonchemistry.cas.org/detail?cas_rn=59729-37-2 | |
| Description | CAS Common Chemistry is an open community resource for accessing chemical information. Nearly 500,000 chemical substances from CAS REGISTRY cover areas of community interest, including common and frequently regulated chemicals, and those relevant to high school and undergraduate chemistry classes. This chemical information, curated by our expert scientists, is provided in alignment with our mission as a division of the American Chemical Society. | |
| Explanation | The data from CAS Common Chemistry is provided under a CC-BY-NC 4.0 license, unless otherwise stated. | |
| Record name | Fexinidazole [USAN:INN] | |
| Source | ChemIDplus | |
| URL | https://pubchem.ncbi.nlm.nih.gov/substance/?source=chemidplus&sourceid=0059729372 | |
| Description | ChemIDplus is a free, web search system that provides access to the structure and nomenclature authority files used for the identification of chemical substances cited in National Library of Medicine (NLM) databases, including the TOXNET system. | |
| Record name | Fexinidazole | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB12265 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | Fexinidazole | |
| Source | EPA DSSTox | |
| URL | https://comptox.epa.gov/dashboard/DTXSID00208448 | |
| Description | DSSTox provides a high quality public chemistry resource for supporting improved predictive toxicology. | |
| Record name | 1-methyl-2-[(4-methylsulfanylphenoxy)methyl]-5-nitroimidazole | |
| Source | European Chemicals Agency (ECHA) | |
| URL | https://echa.europa.eu/information-on-chemicals | |
| Description | The European Chemicals Agency (ECHA) is an agency of the European Union which is the driving force among regulatory authorities in implementing the EU's groundbreaking chemicals legislation for the benefit of human health and the environment as well as for innovation and competitiveness. | |
| Explanation | Use of the information, documents and data from the ECHA website is subject to the terms and conditions of this Legal Notice, and subject to other binding limitations provided for under applicable law, the information, documents and data made available on the ECHA website may be reproduced, distributed and/or used, totally or in part, for non-commercial purposes provided that ECHA is acknowledged as the source: "Source: European Chemicals Agency, http://echa.europa.eu/". Such acknowledgement must be included in each copy of the material. ECHA permits and encourages organisations and individuals to create links to the ECHA website under the following cumulative conditions: Links can only be made to webpages that provide a link to the Legal Notice page. | |
| Record name | FEXINIDAZOLE | |
| Source | FDA Global Substance Registration System (GSRS) | |
| URL | https://gsrs.ncats.nih.gov/ginas/app/beta/substances/306ERL82IR | |
| Description | The FDA Global Substance Registration System (GSRS) enables the efficient and accurate exchange of information on what substances are in regulated products. Instead of relying on names, which vary across regulatory domains, countries, and regions, the GSRS knowledge base makes it possible for substances to be defined by standardized, scientific descriptions. | |
| Explanation | Unless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required. | |
Preparation Methods
Conventional Synthesis of Fexinidazole
The primary synthetic route to this compound, as developed by Hoechst AG (now Sanofi) and later optimized for industrial production, involves a sequence of methylation, hydroxymethylation, chlorination, and coupling reactions.
Methylation of Nitroimidazole
The synthesis begins with the methylation of 5-nitroimidazole (2.1) using dimethyl sulfate in dioxane. This step introduces a methyl group at the N-1 position, yielding 1-methyl-5-nitroimidazole (2.2) with an 82% yield. The reaction proceeds under reflux conditions, with careful control of stoichiometry to minimize byproducts.
Hydroxymethylation
The methylated intermediate (2.2) undergoes hydroxymethylation via treatment with formaldehyde in dimethyl sulfoxide (DMSO). This step introduces a hydroxymethyl group at the C-2 position, producing 2-hydroxymethyl-1-methyl-5-nitroimidazole (2.3) in 62% yield. The use of DMSO as a solvent enhances electrophilic substitution efficiency.
Chlorination
The hydroxymethyl derivative (2.3) is converted to 2-chloromethyl-1-methyl-5-nitroimidazole (2.4) using thionyl chloride (SOCl₂) in chloroform. This step achieves near-quantitative conversion under mild conditions, though the isolated yield is typically limited by purification losses.
Coupling with 4-Methylmercaptophenol
The chlorinated intermediate (2.4) is coupled with 4-methylmercaptophenol (2.5) in the presence of potassium carbonate (K₂CO₃) in acetone. This nucleophilic substitution reaction forms the thioether linkage, yielding this compound hydrochloride (2.6). Neutralization with aqueous ammonia provides the free base, with an overall yield of 65% over the final three steps.
Table 1: Key Steps in Conventional this compound Synthesis
| Step | Reaction | Reagents/Conditions | Yield |
|---|---|---|---|
| 1 | Methylation | Dimethyl sulfate, dioxane, reflux | 82% |
| 2 | Hydroxymethylation | Formaldehyde, DMSO, 60°C | 62% |
| 3 | Chlorination | SOCl₂, chloroform, rt | >90% |
| 4 | Coupling & Neutralization | K₂CO₃, acetone; NH₃(aq) | 65%* |
Isotopic Labeling Techniques
Isotopic labeling of this compound and its metabolites is essential for pharmacokinetic and metabolic studies. Two primary approaches—deuterium (²H) and carbon-14 (¹⁴C) labeling—have been developed.
Deuterium-Labeled this compound
Deuterium incorporation is achieved via base-catalyzed hydrogen-deuterium exchange. Using deuterated solvents (e.g., D₂O) and alkaline conditions, selective deuteration at the methylthio group’s sulfur-adjacent carbon is achieved. This method produces ²H-labeled this compound, sulfoxide, and sulfone metabolites for use as internal standards in liquid chromatography-mass spectrometry (LC-MS).
Carbon-14-Labeled this compound
The ¹⁴C-labeled variant is synthesized via a five-step procedure starting from potassium [¹⁴C]cyanide. The radiolabel is introduced early in the synthetic pathway, ensuring uniform distribution in the final molecule. This labeled compound facilitates absorption, distribution, metabolism, and excretion (ADME) studies.
Optimization of Synthetic Conditions
Solvent and Catalyst Selection
The choice of solvent significantly impacts reaction efficiency. For example, using DMSO in hydroxymethylation enhances electrophilic reactivity compared to polar aprotic solvents like DMF. Similarly, acetone in the coupling step minimizes side reactions compared to higher-polarity solvents.
Analytical Characterization
Nuclear Magnetic Resonance (NMR)
¹H and ¹³C NMR spectra confirm structural integrity. Key signals include:
Comparative Analysis of Synthetic Routes
Table 2: Isotopic vs. Conventional Synthesis
| Parameter | Conventional Route | ¹⁴C-Labeled Route |
|---|---|---|
| Starting Material | Nitroimidazole | K[¹⁴C]CN |
| Key Step | Coupling | Radiolabeling |
| Yield | 65% (overall) | 40–50%* |
| Application | Bulk Production | ADME Studies |
*Estimated from multi-step radiochemical synthesis.
Chemical Reactions Analysis
Types of Reactions: Fexinidazole undergoes several types of chemical reactions, including:
Oxidation: The nitro group can be reduced to an amine under specific conditions.
Substitution: The imidazole ring can undergo nucleophilic substitution reactions.
Hydrolysis: The compound can be hydrolyzed under acidic or basic conditions.
Common Reagents and Conditions:
Oxidation: Common reagents include hydrogen peroxide and metal catalysts.
Substitution: Nucleophiles such as amines or thiols are used.
Hydrolysis: Acidic or basic solutions are employed.
Major Products:
Reduction of the nitro group: results in the formation of an amine derivative.
Substitution reactions: yield various substituted imidazole derivatives.
Hydrolysis: can lead to the breakdown of the compound into simpler molecules.
Scientific Research Applications
Human African Trypanosomiasis
-
Efficacy Against Trypanosoma brucei gambiense :
- Fexinidazole has shown high efficacy in treating early-stage gambiense HAT. Clinical trials demonstrated a cure rate exceeding 90% in patients treated with oral this compound .
- The drug is administered as a 400 mg tablet once daily for 10 days, making it a convenient treatment option compared to previous therapies that required intravenous administration.
- Efficacy Against Trypanosoma brucei rhodesiense :
Safety Profile
This compound has been reported to have a favorable safety profile. In clinical trials, adverse effects were generally mild and manageable, with no severe long-term complications noted . This contrasts sharply with earlier treatments such as melarsoprol, which are associated with significant toxicity.
Comparative Efficacy Data
| Stage of Infection | Treatment Regimen | Cure Rate (%) | Notes |
|---|---|---|---|
| First Stage | This compound (10 days) | >90 | Oral administration; well-tolerated |
| Second Stage | This compound (10 days) | ~91 | Effective against CNS involvement |
| Previous Treatments | Various (IV or IM) | <80 | Often associated with severe side effects |
Case Studies
- Clinical Trial in Democratic Republic of the Congo :
- Pediatric Use :
- Long-term Follow-up :
Mechanism of Action
Fexinidazole exerts its effects by being metabolized into active metabolites that interfere with the parasite’s DNA synthesis. The compound is believed to activate certain enzymes within the parasites, leading to the production of reactive oxygen species that damage the parasite’s cellular structures. This ultimately results in the death of the parasite .
Comparison with Similar Compounds
Pharmacokinetics and Metabolism
Fexinidazole’s pharmacokinetic profile distinguishes it from other nitroimidazoles:
- Rapid absorption : Peak plasma concentrations (Tmax) occur within 0.25–4 hours, with a half-life of 10–16 hours .
- Metabolite-driven efficacy : Sulfoxide and sulfone metabolites contribute to cumulative exposure, enhancing in vivo efficacy compared to single-entity drugs like benznidazole .
- Food interaction : Co-administration with high-fat meals increases bioavailability 3-fold, a critical consideration for patient compliance .
Table 1: Pharmacokinetic Comparison of this compound and Metabolites
| Parameter | This compound | This compound Sulfoxide (M1) | This compound Sulfone (M2) |
|---|---|---|---|
| Free fraction in plasma | 2% | 60% | 43% |
| IC50 (HAT) | 1.0 μM | 0.4–0.8 μM | 0.4–0.8 μM |
| CNS penetration | High | High | High |
| Half-life (h) | 10–16 | 10–16 | 10–16 |
In Vitro and In Vivo Efficacy
Against Trypanosoma cruzi (Chagas disease):
- This compound sulfone achieves >98% parasite clearance in acute murine models at 50 mg/kg twice daily, outperforming benznidazole and nifurtimox .
- However, phase II trials for Chagas were halted due to tolerability issues, highlighting a trade-off between efficacy and safety .
Against Leishmania spp.:
- This compound sulfone and sulfoxide show EC50 values of 0.23–4.4 μM against L. donovani axenic amastigotes, comparable to miltefosine but dependent on nitroreductase activation .
- In murine VL models, 200 mg/kg/day for 5 days reduces parasite burden by 98.4%, mirroring miltefosine’s efficacy .
Table 2: In Vitro Potency Against Key Pathogens
| Compound | T. brucei IC50 | L. donovani EC50 | H. pylori MIC |
|---|---|---|---|
| This compound | 1.0 μM | >50 μM | 5–10 μM |
| This compound sulfoxide | 0.4–0.8 μM | 0.23–3.2 μM | 2.5 μM |
| This compound sulfone | 0.4–0.8 μM | 0.23–3.2 μM | 2.5 μM |
| Miltefosine | N/A | 4.4 μM | N/A |
| Benznidazole | N/A | N/A | N/A |
Mechanism of Action (MoA) and Resistance
- Nitroreductase dependence: this compound’s metabolites require nitroreductase for activation, unlike miltefosine or alkyl phospholipids . Overexpression of nitroreductase in L. donovani increases susceptibility 15-fold .
- Cytocidal vs. cytostatic : this compound sulfone and sulfoxide kill parasites within 30 hours, unlike cytostatic drugs (e.g., azoles), which require prolonged immune support .
Clinical Performance vs. Competitors
Table 3: Clinical Outcomes in Key Indications
| Indication | Compound | Cure Rate (Preclinical) | Clinical Outcome |
|---|---|---|---|
| HAT (Stage 2) | This compound | 100% (murine) | Approved (2018) |
| Chagas (Acute) | This compound | 100% (murine) | Phase II halted (tolerability) |
| Visceral Leish. | This compound | 98.4% (murine) | Phase II relapse observed |
| Visceral Leish. | Miltefosine | >95% (murine) | Approved (oral) |
Sources:
Biological Activity
Fexinidazole is a novel 5-nitroimidazole compound that has garnered significant attention for its potential use in treating human African trypanosomiasis (HAT), also known as sleeping sickness. This disease, caused by the protozoan parasites Trypanosoma brucei gambiense and Trypanosoma brucei rhodesiense, poses a considerable health risk in sub-Saharan Africa. This compound is unique as it is the first oral treatment approved for HAT, providing a much-needed alternative to existing therapies that often require intravenous administration.
This compound acts as a prodrug, requiring metabolic activation to exert its therapeutic effects. Upon administration, it undergoes two-electron reduction to form two primary active metabolites: this compound sulfoxide and this compound sulfone. These metabolites are responsible for the compound's trypanocidal activity against various strains of T. brucei.
In Vitro and In Vivo Efficacy
Research has demonstrated the efficacy of this compound and its metabolites in both in vitro and in vivo settings. The following table summarizes key findings regarding the biological activity of this compound against T. brucei:
Pharmacokinetics
This compound exhibits favorable pharmacokinetic properties, characterized by rapid absorption and metabolism. Key pharmacokinetic parameters after oral administration in mice include:
- Cmax :
- This compound: 500 ng/mL
- Sulfoxide: 14171 ng/mL
- Sulfone: 13651 ng/mL
- AUC (0-24 hours) :
- This compound: 424 h.ng/mL
- Sulfoxide: 45031 h.ng/mL
- Sulfone: 96286 h.ng/mL
These data indicate that the metabolites contribute significantly to the therapeutic effect observed in vivo, with prolonged exposure enhancing efficacy against T. brucei.
Clinical Trials
This compound has undergone extensive clinical trials, demonstrating its safety and effectiveness in treating HAT. The pivotal study included patients with both early and late-stage disease, showing a high cure rate and minimal side effects compared to traditional therapies.
Comparative Studies
In comparative studies against established treatments like eflornithine and nifurtimox, this compound has shown comparable efficacy but with the added benefit of oral administration, which improves patient compliance and reduces healthcare costs associated with intravenous therapies.
Q & A
Basic Research Questions
Q. What methodologies are recommended for designing preclinical studies to evaluate Fexinidazole’s efficacy against African trypanosomiasis?
- Use validated animal models like the GVR35 chronic murine model, which correlates plasma concentrations of this compound’s sulfone metabolite (M2) with curative outcomes . Ensure pharmacokinetic (PK) parameters (e.g., time to steady state, bioavailability) align with human trial data. Include control groups for comparison and measure M2 levels in cerebrospinal fluid to assess CNS penetration .
Q. How should researchers address food interaction effects in this compound dosing studies?
- Conduct randomized crossover trials comparing bioavailability under fasted vs. fed conditions (e.g., high-fat vs. carbohydrate-rich meals). Use PK modeling to simulate absorption rates and adjust dosing regimens. For example, Study Protocol 2 (NCT01340157) demonstrated that food type significantly impacts bioavailability, requiring adjustments in clinical protocols .
Q. What strategies ensure reproducibility in this compound pharmacokinetic studies?
- Standardize protocols for blood sampling, metabolite quantification (e.g., LC-MS/MS), and data reporting. Include detailed descriptions of renal clearance rates, free drug fractions, and inter-subject variability in supplementary materials. Reference in vitro data (e.g., protein binding assays) to validate human findings .
Advanced Research Questions
Q. How can population pharmacokinetic modeling optimize this compound dosing in heterogeneous populations?
- Integrate data from Phase I trials (e.g., Study Protocol 3, NCT0148370) to build nonlinear mixed-effects models. Incorporate covariates like body weight, hepatic function, and genetic polymorphisms in CYP450 enzymes. Validate simulations against murine efficacy thresholds (e.g., M2 >10,000 ng/mL for 24h) .
Q. What analytical frameworks resolve contradictions between preclinical and clinical efficacy data for this compound?
- Apply meta-analytical techniques to compare murine and human PK/PD relationships. For discrepancies in CNS penetration, use compartmental modeling to adjust for blood-brain barrier variability. Cross-reference safety data (e.g., Holter ECG results) to identify confounders like cardiac toxicity .
Q. How should researchers design studies to compare this compound with nifurtimox-eflornithine combination therapy?
- Use adaptive trial designs with primary endpoints like parasite clearance time and relapse rates. Stratify participants by disease stage (early vs. late) and monitor adverse events (AEs) via blinded safety review committees. Leverage literature review methodologies (e.g., PubMed search filters) to identify comparator trial protocols .
Retrosynthesis Analysis
AI-Powered Synthesis Planning: Our tool employs the Template_relevance Pistachio, Template_relevance Bkms_metabolic, Template_relevance Pistachio_ringbreaker, Template_relevance Reaxys, Template_relevance Reaxys_biocatalysis model, leveraging a vast database of chemical reactions to predict feasible synthetic routes.
One-Step Synthesis Focus: Specifically designed for one-step synthesis, it provides concise and direct routes for your target compounds, streamlining the synthesis process.
Accurate Predictions: Utilizing the extensive PISTACHIO, BKMS_METABOLIC, PISTACHIO_RINGBREAKER, REAXYS, REAXYS_BIOCATALYSIS database, our tool offers high-accuracy predictions, reflecting the latest in chemical research and data.
Strategy Settings
| Precursor scoring | Relevance Heuristic |
|---|---|
| Min. plausibility | 0.01 |
| Model | Template_relevance |
| Template Set | Pistachio/Bkms_metabolic/Pistachio_ringbreaker/Reaxys/Reaxys_biocatalysis |
| Top-N result to add to graph | 6 |
Feasible Synthetic Routes
Featured Recommendations
| Most viewed | ||
|---|---|---|
| Most popular with customers |
Disclaimer and Information on In-Vitro Research Products
Please be aware that all articles and product information presented on BenchChem are intended solely for informational purposes. The products available for purchase on BenchChem are specifically designed for in-vitro studies, which are conducted outside of living organisms. In-vitro studies, derived from the Latin term "in glass," involve experiments performed in controlled laboratory settings using cells or tissues. It is important to note that these products are not categorized as medicines or drugs, and they have not received approval from the FDA for the prevention, treatment, or cure of any medical condition, ailment, or disease. We must emphasize that any form of bodily introduction of these products into humans or animals is strictly prohibited by law. It is essential to adhere to these guidelines to ensure compliance with legal and ethical standards in research and experimentation.


